Hemoglobin Structure and function Flashcards
Describe the structure of hemoglobin:
What is the heme group linked to each hemoglobin cahin called?
- Tetramer
- Composed of two unlike pairs of globin polypeptide chains (mostly alpha and beta chains in the normal adult).
- With a heme group (ferroprotoporpyrin IX) linked covalently to each chain (via histidine)
Primary role: oxygen delivery

In what state shoud Iron be to bind oxygen?
What is methemoglobin?
What enzyme reduces ferric to ferrous iron?
- Iron needs to be in reduced form (ferrous; Fe+2) to bind oxygen.
- When in oxidized form (ferric; Fe+3), iron can’t bind oxygen.
–>Hemoglobin with iron in ferric form is called methemoglobin.
•Iron is reduced from ferric to ferrous form by cytochrome b5 reductase.
What is the deoxygenated hemoglobin state called?
What is the Relax conformation of hemoglobin?
•Deoxygenated hemoglobin is in a Taut (T) conformation due to salt bonds, hydrogen bonding, and hydrophobic interactions
•With binding to oxygen, the bonds progressively break, and the hemoglobin converts to a Relaxed (R) conformation
What is allostery?
If the allosteric changed lead to increase affinity for substrate, this called______ and is seen in hemglobin.
- Allostery: substrate binding at one site on a protein leads to altered confirmation at other binding sites on the protein.
- If the allosteric changes lead to increased affinity for substrate at the other binding sites, it is termed positive cooperativity.
Oxygen dissociation curve for hemoglobin (HB A1):
What determined the Sigmoidal shape of the curve:
What is the meaning if the curve?

As you increase the partial pressure of O2 you increase the affinity of hemoglobin for O2.
Cooperativity determines the sigmoidal shape.
•Allows oxygen to easily bind at higher pO2 level in lungs and unload at lower pO2 level in tissues.
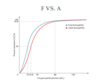
Hemoglobin vs. Myoglobin curves
What is P50 in terms of the oxygen dissociation curve?


What factors shift the oxygen dissociation curve to the right?
What causes a left-shift)
A right shift of the ODC curve means that the oxygen affinity has decreased (which could be beneficial in terms of providing oxygen to tissues in situation of anemia or hypoxia).
Factors:
1) Decrease pH
2) Increased temperature
3) Increase 2,3-BPG
A left-shift means increase affinity for Oxygen by hemoglobin.
Factors that cause it: 1) Increased temperature, decreased 2,3-BPG, Increased pH.

What is the Bohr effect?

How does CO2 affects the oxygen dissociation curve?

How does temperature affects the ODC?

What is the effect of 2,3-BPG?

2,3‐bisphosphoglycerate (2,3‐BPG), also known as 2,3‐diphosphoglycerate or 2,3‐DPG, is a byproduct of the anaerobic glycolytic pathway and is normally present in red cells at a concentration of ~5 mmol/L. When the level is higher, such as occurs during states of increased oxygen utilization and glycolysis, chronic hypoxia, and chronic anemia, oxygen affinity of hemoglobin decreases and shifts the curve to the right, increasing delivery of oxygen to tissues. 2,3‐BPG alters oxygen affinity by binding to (in between B chains) deoxyhemoglobin and stabilizing it in the T configuration, leading to decreased affinity of the hemoglobin for oxygen.



In terms of hemoglobin, how does the neonate differ from an adult?

What is special aboit hemoglobing produced in the embryo?
The are a higher affinity hemoglobins produced in the embryo.
–>Allow preferential uptake of oxygen by the placenta from the maternal circulation.
What is fetal hemoglobin?
At what point does it start dominating in terms of production?
Does it have a higher or lower affinity for oxygen than Hb?
Does it bind 2,3-BPG?
•α2γ2
Dominates after week 8 of gestation
- With higher affinity for oxygen (left shifted curve) than HbA
- Hemoglobin F doesn’t bind 2,3-BPG as well
–>More pronounced Bohr effect