Anemis due to decreased cell production Flashcards
For folate and vitamin B12 deficiencies, what are the MCV indices?
What type of anemia is it considered?
MCV>100, which means cells are macrocytic
Considered an underproduction anemias
–>Megaloblastic anemias
How is folate and vit B12 required for DNA synthesis?
Methionine is synthesized from?
What is a substrate for purine and pyrimidine?
What compound is required for normal DNA synthesis?
Folic acid and vitamin B12 (cobalamin) are critical co-factors for normal hematopoiesis.
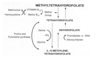
Methyltetrahydrofolate (a metabolite of folic acid) is a methyl group donor and essential co-factor, along with vitamin B12, in the synthesis of methionine from homocysteine. This reaction generates tetrahydrofolate which is a substrate for purine and pyrimidine synthesis and the conversion of deoxyuridylate to **thymidylate (required for normal DNA synthesis).
Deficiencies in Vit B12 and folate affect what?
What is nuclear-cytoplasmic dyssinchrony?
Deficiencies of folic acid and vitamin B12 profoundly affect the maturation process of red cell precursors in the marrow.
The cells increase in size (macrocytic), arrest in S phase of mitosis, and then undergo destruction, resulting in ineffective erythropoiesis and anemia.
Nuclear-cytoplasmic dyssinchrony refers to: The impaired nuclear maturation is seen as open, loose, immature chromatin (cut-salami pattern). In contrast to the nucleus, the cytoplasm of megaloblastic cells is abundant with normal hemoglobinization. This disparity between nucleus and cytoplasm is known as nuclear-cytoplasmic asynchrony.

In what foods can you find vit B12?
Is vit B12 used by plants?
What is the process of absorption for vit B12?
Vitamin B12 is synthesized by bacteria and algae, eventually working its way up the food chain to humans through consumption of meat, eggs, and milk.
It is required as a vitamin by animals but not by higher plants - hence, plants do not contribute Vitamin B12 to the diet, and a strict vegan diet can lead to deficiency.
Once ingested, Vitamin B12 in food is released in the acid environment in the stomach.
1) The protein carrier, intrinsic factor (IF), is secreted by gastric parietal cells and binds vitamin B12.
2) In the terminal ileum, the IF-B12 complex is absorbed and B12 released from IF, bound to transcobalamin binding protein II (TcII) and transported to the liver for storage or to other tissues like the bone marrow for use.

Is it common for vit B12 deficiency to occur due to dietary intake?
What is pernicious anemia?
It is unusual for Vitamin B12 deficiency to be caused by inadequate dietary intake.
The most common cause of Vitamin B12 deficiency is pernicious anemia, due to autoimmune destruction of IF-producing gastric parietal cells. This condition is most common in the older age population. Other causes include failure to produce IF (gastritis, gastrectomy, congenital), malabsorption (multiple disorders), defective transport or storage (TcII deficiency) and metabolic defects in pathways which utilize B12 as a substrate.

Neurologic involvement is characteristic of?
What neurological issues occur at first?
As the deficiency progresses what other symptons can you observe?
Are neurologic problems completely reversible after vit B12 administration?
Why is it important to rule out vit B12 deficiency?
Neurologic involvement is classic in B12 deficiency, though it can less frequently be seen in folate deficiency.
- Sensory abnormalities (numbness, tingling, loss of fine sensation) occur first. Loss of proprioeption (perception of movement and spacial orientation) may also be documented.
- As the deficiency progresses, ataxia (gross lack of coordination of muscle movements), spasticity**, **gait disturbances**, and a positive **Babinski reflex (in response to stroking of the sole of the foot, extension rather than flexion of the great toe) may follow.
- Sometimes cerebral signs are seen including cognitive dysfunction and emotional changes.
Anemia may be absent in 28% of patients with neurologic problems.
Neurologic defects may not be completely reversible after B12 administration.
If a patient with undiagnosed B12 deficiency is treated with large doses of folic acid, neurologic damage can be exacerbated, making it critical to rule out B12 deficiency before initiating treatment with folic acid.

What is the Schilling test used for?
How is it performed?
What is a cold dose?
How do you read the test?
How can you diagnose anemia based on the Schillings Test?
The Schilling test is an older test used to diagnose defects in B12 absorption that is less commonly used today but still important to know about.
In this test, 1 μg of radiolabeled cobalamin is given orally to a fasting individual. The IF produced in the stomach combines with the radiolabeled cobalamin (Cbl) which is absorbed in the terminal ileum. The tagged cobalamin is then bound to transcobalamin II (TcII) and enters the bloodstream. Then, a dose of cold (unlabeled) cobalamin is given intramuscularly 2 hours later, causing some of the labeled cobalamin to be excreted in the urine over the following 24 hours (5-35%). If the patient isn’t absorbing the cobalamin given orally, less radiolabeled cobalamin will be excreted into the urine.
How to read results?
- Decreased urine excretion of radiolabeled B12 –> decreased absorption
- Normal urine excretion of radiolabeled B12 –> decreased dietary intake
- Test can be repeated with concomittant IF administration to diagnose pernicious anemia.

In which foods can you find folate?
Can you give goat milk to your kid?
Where is folate absorbed?
How does the liver prodices a constant supply to the tissues?
Folate is widespread in food. With a typical diet, about one third of the daily folate intake is provided by cereals and bread, another one third by fruits and vegetables, and the remaining one third by meats and fish. Human milk provides enough folate for infants.
Goat’s milk, however, contains little folate, and children maintained on it alone can develop severe deficiency.
Overcooking can also lead to loss of folates in food. Dietary folate is absorbed in the jejunum. It is hydrolyzed, reduced and methylated before distribution to the tissues or liver for storage (as methyltetrahydrofolate).
-The liver stores undergo turnover, secretion in the bile and reabsorption (enterohepatic circulation) supporting a constant supply to tissues.
What is the most common cause of folate deficiency?
What other factors can decrease folate?
Can alcohol lead to folate deficiency?
In contrast to B12 deficiency, the most common cause of folate deficiency leading to megaloblastic anemia is inadequate dietary intake.
Other causes include malabsorption due to such things as gluten sensitivity or parasitic infection, which can lead to rapid depletion of folate through interruption of enterohepatic circulation.
Inborn errors of folate metabolism (very rare).
Increased demands (hemolysis, pregnancy/lactation, rapid growth, psoriasis, myeloproliferative disorders).
-Alcohol consumption also can lead to rapid onset of folate deficiency, not only through decreased dietary intake but also through disruption of cycling from liver stores to tissues.
Table with differences between folate and vit B12:

What are the differences in onset of folate and vit B12 deficiency?
Both folic acid and vitamin B12 deficiency result in megaloblastic anemia.
The onset of folate deficiency can occur quite rapidly (within weeks), particularly in the setting of malabsorption or alcoholism.
In someone who is well-nourished, Vitamin B12 deficiency takes several months to develop because of its long half-life within the body and large hepatic stores. Vitamin B12 deficiency develops more slowly and can also be associated with malabsorption. The symptoms and signs of anemia in both cases are not distinguishable from other causes.
What hematologic changes can be observed?
-In the bone marrow, erythroid hyperplasia leading to an alteration of the myeloid:erythroid (M:E) ratio from a myeloid to an erythroid predominance is observed.
-Megaloblastic changes are seen in both erythroid and myeloid series.
- Cytoplasmic maturation is normal but at any stage of the development, marrow precursors show large, immature nuclei (termed nuclear-cytoplasmic asynchrony).
- In peripheral blood, the anemia is variable.
- There is macrocytosis (MCV >97 fl in adults).
- The reticulocyte count is decreased, with a reticulocyte index <1.0.
- On the peripheral smear, macro-ovalocytes and hyper-segmented (≥4-5 lobes) neutrophils can be observed.
- As the anemia progresses, poikilocytes and fragmentation may be seen. In severe cases, neutropenia and thrombocytopenia can be documented, as well as increases in bilirubin and LDH levels due to intramedullary (within the bone marrow) destruction of red cells.

What problems exist in measuring serum cobalamin and folate levels?
What is a more sensitive marker for testing deficiency in vit B12 and folate?
What reaction involves vit B12 but not folate?
Direct measurement of serum cobalamin levels and serum or red cell folate levels is useful in diagnosing deficiencies, although there can be problems with these tests.
-Cobalamin deficiency in the tissues can exist with a normal serum cobalamin level.
Serum folate levels may reflect recent intake and not tissue stores, while red cell folate is a better indicator of tissue folate status but may be low with B12 deficiency.
-Measurement of plasma homocysteine levels has been used as a more sensitive marker of deficiency of B12 and folate in the tissues. As indicated in the metabolic pathways described above, vitamin B12 and folic acid are both required for the synthesis of methionine from homocysteine.
So, deficiency of either one of these vitamins should lead to elevated homocysteine levels.
Another reaction involving vitamin B12 but not folate is the synthesis of succinyl CoA from methylmalonyl CoA. Thus, in vit B12 but not folate deficiency, methylmalonic acid levels are increased, making measurement of methylmalonic acid a good way to distinguish the two.

Treatment of folate and cobalamin (vit B12) deficiencies:

What are the characteristics of normocytic anemias?
MCV 80-100
Anemia of chronic disease
Renal disease
Hypo/hyperthyroidism








