Physiology of the Heart Flashcards
Used to describe a collection of mechanisms that influence the active and changing circulation of blood circulation of different volumes of blood per minute at different times is essential for survival
hemodynamics
the circulation control mechanisms must accomplish 2 function:
- maintain circulation (keep blood flowing) - Vary volume and distribution of the blood circulated
A complete heartbeat, or pumping cycle, consisting of contraction (systole) and relaxation (diastole) of both atria and both ventricles
the cardiac cycle
contraction of both ventricles of the heart, forcing blood out of these chambers. The atria are in a relaxed state
systole
The top number of BP, which is also the higher of the 2 numbers, measures the pressure in the arteries when the heart beats (contracts)
systolic
The bottom number, which is also the lower of the 2 numbers, measures the pressure in the arteries between heartbeats (when heart muscle is resting between beats and refilling with blood)
diastolic
ventricular muscles relax, allowing for blood to fill these chambers. At the end, the atria start contracting to fill the ventricles
diastole
an electrical fluctuation that travels along the surface of a cell’s membrane mediated by the flow of sodium and potassium ions across the membrane; occurs in nerves and muscles.
action potential
- repeatedly generate action potentials that trigger contraction and continue to stimulate heart even after it has been removed from the body
autorhythmic cardiac muscle fibers
_____, _____, and _____ can alter heartbeat strength and heart rate, but do not change the coordinated contractions of the heart
hormones, chemicals, and nerve impulses
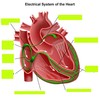
Conduction system of the heart has 4 structures:
- sinoatrial (SA) node - Atrioventricular (AV) node - AV bundle (bundle of His) - subendocardial branches (purkinjie fibers)
- The natural or inherent “pacemaker” of the heart - Initiates each heartbeat and and sets it pace - located high in r atrial wall
sinoatrial node
impulses spread from the ______ to the muscle fibers of both atria causing atrial contraction
SA node
The _____ fires between 60-100 BPM
SA node
- Located at the base of the right atrium - electrically, it acts as the only gateway for electrical impulses from the atria to the ventricles
Atrioventricular node (AV)
electrical activity travels very slowly through the _______. The delay allows for contraction of the atria to proceed contraction of the ventricles.
AV node
AV node stimulation sends impulses to the ________.
atrioventricular bundle of His
carries electrical impulses (action potentials) into the ventricles. Impulses travel through the right and left bundle branches to the Purkinjie fibers.
bundle of His
fibers that further spread electrical activity to all parts of the ventricles so that there is a coordinated contraction of each ventricle.
subendocardial branched AKA Purkinjie fibers
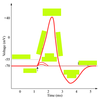
a graphic record of the heart’s electrical activity, specifically the conduction of impulses. It is not a record of the heart’s contractions, but of the electrical events/current that precede them a composite record of action potentials produced by the heart muscle fibers during each heartbeat.
electrocardiogram (ECG)
In an ECG, changes in voltage are seen as _______ of a line drawn on a paper or traced on a video monitor.
deflections
The _______ is composed of deflection waves called the P wave, QRS complex, and T wave.
normal ECG
A _______ obtains 12 electrical tracings of the heart from different angles or orientations. Patterns of abnormalities can indicate areas of abnormal conduction.
12-lead ECG
represents depolarization of the atria. Deflection related to passage of an electrical impulse from the SA node through the muscle of both atria.
The P wave
larger _______ indicate enlargement of an atria.
P waves