DI Midterm Exam Material Flashcards
T/F: Pneumomediastinum may result in dyspnea
False
If you see an enlargement in this region, what should your top two differentials be?

Tracheobronchial lymphadenopathy and Left atrial enlargement

T/F: Ring Shadows (donuts) are often associated with a bronchial pattern
True
Bronchial pattern: donuts and tram lines
T/F: Hepatic veins have a hyperechoic wall on ultrasound
False
Hepatic veins have an isoechoic wall
This is a sagittal image of the left kidney. Which side is cranial?

That one.

What view would be best for evaluating lesions in the right lung lobes?
Left Lateral
- In small animals, lung lesions generally are detected best in the non-dependent lung because the “up” lung is better aerated and therefore provides better contrast of lesions*
- Keep in mind, other lesions (not in the lung) generally are best seen on the “down” side because they are not distorted by magnification*
What echocardiographic modality would you use to measure wall thickness during systole and diastole?
M Mode
Name the MR sequence that nulls signal from free fluid (i.e. CSF):
FLAIR
_FL_uid _A_ttenuated _I_nversion _R_ecovery
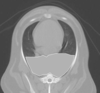
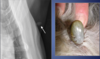
Is sternal lymphadenopathy present in this patient?

Yes.
Note the enlargement of the sternal lymph node

T/F: Ascites is commonly associated with mitral valve insufficiency
False
That is false
Is the circled lesion more likely in the lung or the mediastinum?

Lung
Note the acute angle to the body wall. If the lesion was in the lung you would not have such an acute angle
With which radiographic view is mediastinal shift best visualized?
VD/DV
Doppler measurements should be taken with the patient in ______ lateral recumbency
LEFT
If you see a “bow-legged cowboy sign” on a DV view, what is your DDx?

left atrial enlargement

Identify the lymphatic structure indicated by the number 3:

Tracheobronchial

T/F: Diaphragmatic hernias cause caudal displacement of the gastric axis
False
Diaphragmatic hernias cause cranial displacement of the gastric axis
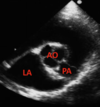
Long-axis left ventricular outflow view.
Identify the structure indicated by the number 2

right atrium

T/F: An overexposed radiograph is too light
False
An overexposed radiograph is too dark. Either kVp or mAs is too high.
T/F: If you suspect a lesion in the right lung of a dog, a left lateral thoracic radiograph should be made
True
What diagnostic imaging modalities might you use if you suspect a diaphragmatic hernia?
Radiographs, Ultrasound, Barium Study
RUB the hernia…
…creep
T/F: Atelectasis is associated with normal to increased size of the lung lobe
False
- Atelectasis is associated with decreased size of the lung lobe*
- Consolidation is associated with normal to increased size of the lung lobe*
This presentation is most often associated with _______ insufficiency

mitral insufficiency
Turbulent flow (regurgitation); often bright and a mixture of colors
T/F: Mammary adenocarcinomas are typically associated with mediastinal lymphadenopathy
False

T/F: Tracheobronchial lymphadenopathy is an example of a cranioventral disease
False
Tracheobronchial lymphadenopathy is an example of a dorsal disease
T/F: Pneumothorax may progress to pneumomediastinum
No!
Pneumomediastinum may progress to pneumothorax, but not the other way around
When using grids for radiographs, how should you adjust the mAs?
Increase mAs
The grid ‘intercepts’ scatter from patient before it reaches film. You need 2x-3x more photons when grid is used (higher mAs) due to absorption of primary beam by lead
If you suspect a right lung lesion, what radiographic views would you take for the dog? What about a horse?
Dog: R → L
Horse: L → R
Which has better contrast resolution: flat panel or film?
Flat panel
Identify the cardiac abnormality:

Pericardial Effusion
T/F: The cranial vena cava is normally visible radiographically in the mediastinum
False

T/F: Decreased mAs would contribute to increased film blackness
False
Increased mAs would increase film blackness
T/F: A diagnosis of cardiac failure can not be based on echocardiology alone
True
Are mediastinal masses typically more evident in a lateral view or a ventrodorsal view?
ventrodorsal (VD) view
T/F: The esophagus is normally visible on survey radiographs
FALSE
The esophagus is normally not visible on survey radiographs
What is the most common vascular ring anomaly?
Persistent right fourth aortic arch
If the distance between the film and the x-ray source decreases from 40” to 30”, how much does radiation intensity at the film change?
By 402/302
Intensity of radiation (x-rays/unit area) decreases with the square of the distance from the source
Identify the structure indicated by the red star:
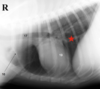
caudal vena cava

This “scalloping” appearance of the lung margins indicates:
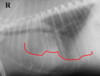
pleural effusion
Identify the lymphatic structure indicated by the number 2:

Cranial Mediastinal

For thoracic radiographs, what should your mAs and kVp settings be?
high kVp, low mAs
_________ is the extent to which a film, image plate or flat panel can be over and underexposed and still acheive an acceptable result
Exposure latitude
Identify the structure indicated by the red star:

right middle lung lobe

Is pneumomediastinum present in this radiograph?

Yes
Normally all of the tubular structures arent so readily visible, but in the case of pneumomediastinum gas acts as a contrast agent and allows for visualization of structures that would normally be undetected
Is this radiograph under-exposed or over-exposed?

Over-exposed
To correct this radiograph, you could decrease the mAs or decrease the kVp
The number of x-rays produced in a radiograph is quantified as:
mAs
T/F: Doubling the mAs doubles the amount of x-rays produced
True
Of the many structures present in the mediastinum of the normal thorax, only a few structures are seen radiographically.
Name ‘em, biatch!
- Heart
- Aorta
- Trachea
- Thymus (young animals)
- Caudal vena cava
- Occasionally Esophagus (left lateral)
“_H_ere _A_re _T_he _T_hings _C_ommonly _O_bserved” in the mediastinum
T/F: Border effacement is often associated with a bronchial pattern
False
Border effacement is associated with alveolar patterns
T/F: The diaphragm attaches to the ventral aspect of L3-L4
True
Pectus excavatum: detected or not detected?
Detected
Pectus excavatum is dorsal displacement of the sternum. It often results in narrowing of the thorax and is often associated with respiratory and CV anomalies
A change of kVp by _______ is equivalent to halving or doubling mAs
16-20%
Identify the lymphatic structure indicated by the number 1:

Sternal

If you see an interstitial pattern, is that considered airway or non-airway disease?
Non-airway

T/F: Grids are often used in radiography when the patient is less than 10 cm thick
False
Grids are often used in radiography when the patient is more than 10 cm thick. (Thicker patients create more scatter)
Which one of these radiographs is normal?
What do you observe in the abnormal one?

B is normal
In A, you can observe air bronchogram (this is indicative of an alveolar pattern) - there is air in the bronchus and the alveoli are filled with fluid. You can also observe border effacement, sillhouetting of the cranial margin of the heart.

Long-axis left ventricular outflow view.
Identify the structure indicated by the number 1

right ventricle